Researchers have identified a novel antibiotic molecule targeting Mycobacterium tuberculosis, reducing its pathogenicity to humans. Additionally, some discovered substances may allow the re-treatment of tuberculosis, including strains that have developed resistance to existing drugs.
The findings were published in the journal “Cell Chemical Biology” under the title “Discovery of Dual-Action Ethionamide Boosters Inhibiting the ESX-1 Secretion System of Mycobacterium tuberculosis.”
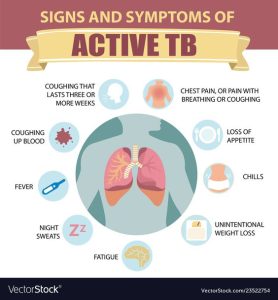
Tuberculosis (TB), formerly known as “consumption,” primarily affects the lungs but can also damage other organs. With early diagnosis and antibiotic treatment, it can be cured. Although relatively rare in most Western countries, TB remains one of the world’s deadliest infectious diseases.
According to the World Health Organization (WHO), in 2022, only COVID-19 was more lethal than tuberculosis. The death toll from TB is nearly double that of HIV/AIDS. Over 10 million people still contract tuberculosis annually, largely due to inadequate access to medical services in many countries.
Limited Targets
Multidrug-resistant tuberculosis is on the rise, especially in Eastern Europe and Asia. Researchers are particularly concerned because Mycobacterium tuberculosis, like all bacteria infecting humans, has a limited number of targets for conventional antibiotics. This makes discovering new antibiotic substances in the laboratory increasingly challenging.
Researchers from the University Hospital of Cologne collaborated with colleagues from the Institut Pasteur in France and the German Center for Infection Research (DZIF) to identify alternative treatment strategies for this bacterium. The team utilized a host-cell-based high-throughput approach to test the molecules’ ability to inhibit bacterial growth within human immune cells. Out of 10,000 molecules, this process allowed them to isolate a few molecules for more detailed examination.
Dual Attack
Ultimately, researchers identified a virulence inhibitor with a target structure fundamentally different from the targets of conventional antibiotics.
“These molecules could significantly reduce selective pressure on bacteria, thereby decreasing resistance,” said Jan Rybniker, Head of the Department of Infectious Disease Translational Research at the Cologne Center for Molecular Medicine (CMMC), who initiated the study.
While deciphering the exact mechanism of action, researchers also found some newly discovered chemical substances to be dual-active molecules. Hence, they not only target the pathogen’s virulence factors but also enhance the activity of monooxygenase, an enzyme required for the activation of the traditional antibiotic ethionamide.
Ethionamide has been used for decades to treat tuberculosis. It is a prodrug, a substance that needs activation by enzymes in bacteria to kill them. Therefore, the discovered molecules serve as prodrug enhancers, offering an alternative approach to developing traditional antibiotics.
Collaborating with the research team led by Professor Alain Baulard at the University of Lille, the precise molecular mechanism of this boosting effect was deciphered. Thus, drugs already used to treat tuberculosis might continue to be effective in the future when combined with these new active substances.
This discovery provides several attractive starting points for developing new and urgently needed tuberculosis drugs.
“Furthermore, our work is an intriguing example of the pharmacological diversity of active substances. The activity spectrum of these molecules can be modified with minimal chemical alterations,” added Rybniker. However, applying these findings to humans is a long process, requiring extensive adjustments to the substances in the laboratory.
